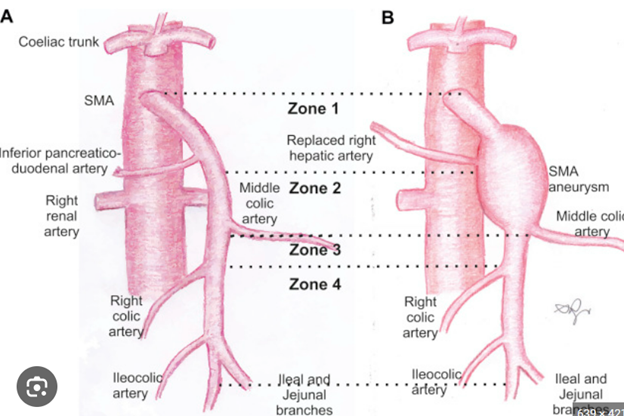
What Are Visceral Aneurysms?
Visceral aneurysms are aneurysms that occur in the arteries supplying blood to the internal organs.
These include:
- Splenic artery (spleen)
- Hepatic artery (liver)
- Renal artery (kidney)
- Mesenteric arteries (intestines)
These aneurysms are relatively rare, and most are discovered incidentally during imaging for unrelated issues. Because they rarely cause symptoms until rupture, early identification is critical. Occasionally, patients may feel vague abdominal pain, but most have no warning signs.
- Which artery is involved
- How large the aneurysm is
- What the specific risks are
Diagnosing and Monitoring Visceral Aneurysms
- Confirm the diagnosis using high-resolution vascular imaging (CT angiography)
- Assess aneurysm size, shape, and location
- Determine the risk of rupture and candidacy for repair
- Begin surveillance with serial imaging and clinic visits if the aneurysm is small and stable
When Is Treatment Needed?
We consider treatment when:
- The aneurysm reaches a critical size threshold (which varies by artery)
- There is evidence of growth
- It is symptomatic or discovered in high-risk situations (e.g., pregnancy with splenic artery aneurysm)
- There are signs of impending rupture
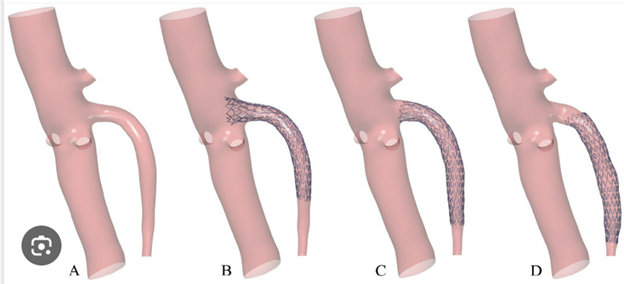
Minimally Invasive Treatment Options
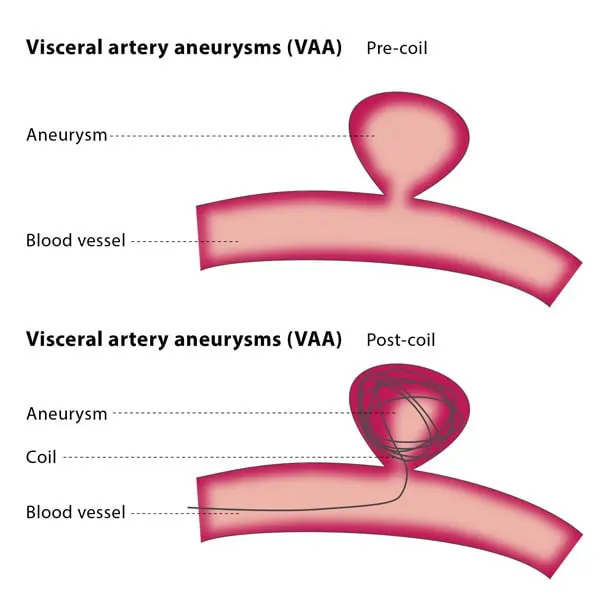
Whenever possible, we use endovascular techniques, which allow us to treat the aneurysm through a small puncture in the groin or arm—avoiding large incisions and lengthy recovery.
Endovascular Techniques Include:
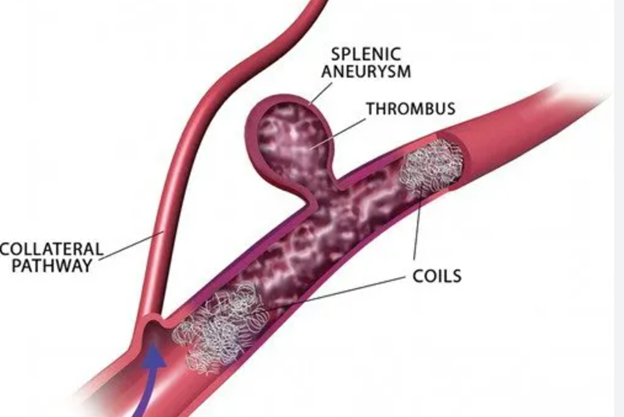
- Coil Embolization: Metal coils are placed inside the aneurysm to clot it off and prevent rupture (commonly used for splenic artery aneurysms).
- Covered Stent Grafting: A stent with an inner graft lining is used to reroute blood flow through the artery, excluding the aneurysm.
- Coil Embolization and stent placement: Combination techniques for complex branch aneurysms, such as in the renal arteries or mesenteric vessels.
Key Advantages:
- Performed under image guidance
- Usually requires only overnight hospital observation
- Faster recovery, often with only minor soreness at the access site
- Comparable outcomes to open surgery with fewer complications
Surgical Repair: When Endovascular Isn’t Enough
- Ligation (tying off the artery)
- Bypass or reconstruction to restore blood flow
What to Expect
- Imaging review and risk assessment
- Clinic consultation to discuss treatment plan
- Blood tests or additional imaging if needed
- Most endovascular cases are done with local anesthesia and mild sedation
- Procedure length varies by location and technique
- Small puncture access (groin or arm)
- Usually one night stay in the hospital for observation
- Return to activity within a few days for endovascular repair
- Continued imaging surveillance and clinic visits to ensure long-term success and stability
Frequently Asked Questions
Are visceral aneurysms dangerous?
They can be. While many remain stable, some can rupture unexpectedly—especially splenic or mesenteric aneurysms. That’s why timely diagnosis and careful planning are essential.
How do you decide which treatment to use?
We assess your artery, aneurysm size, shape, and location to determine whether embolization, stent grafting, or surgery is most appropriate.
Will I need long-term follow-up?
Yes. We schedule serial imaging and routine clinic visits to monitor for regrowth, new aneurysms, or rare complications.
Is recovery easier with endovascular treatment?
Yes. Most patients recover rapidly after coil embolization or stent graft placement, with minimal downtime and low risk of complications.
Why Choose Vascular Clinic?
- Expertise in Rare and Complex Aneurysms
- Minimally Invasive Endovascular Specialists
- Customized Approach for Each Artery and Aneurysm
- Onsite Imaging, Diagnosis, and Long-Term Surveillance
- Compassionate, Clear Communication at Every Step