What Is Renal Artery Disease?
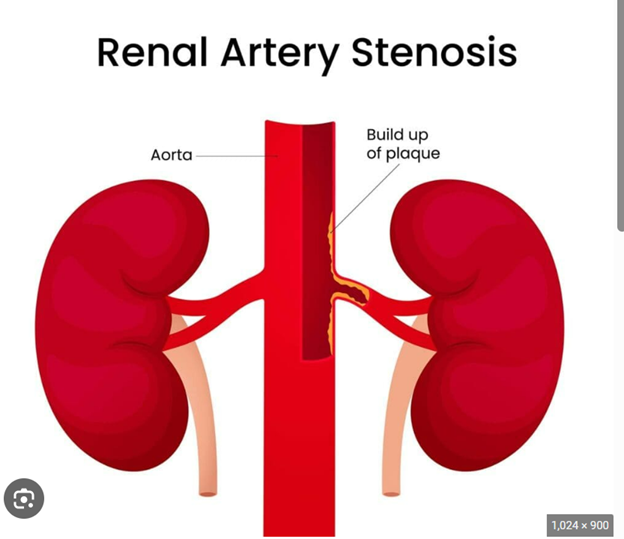
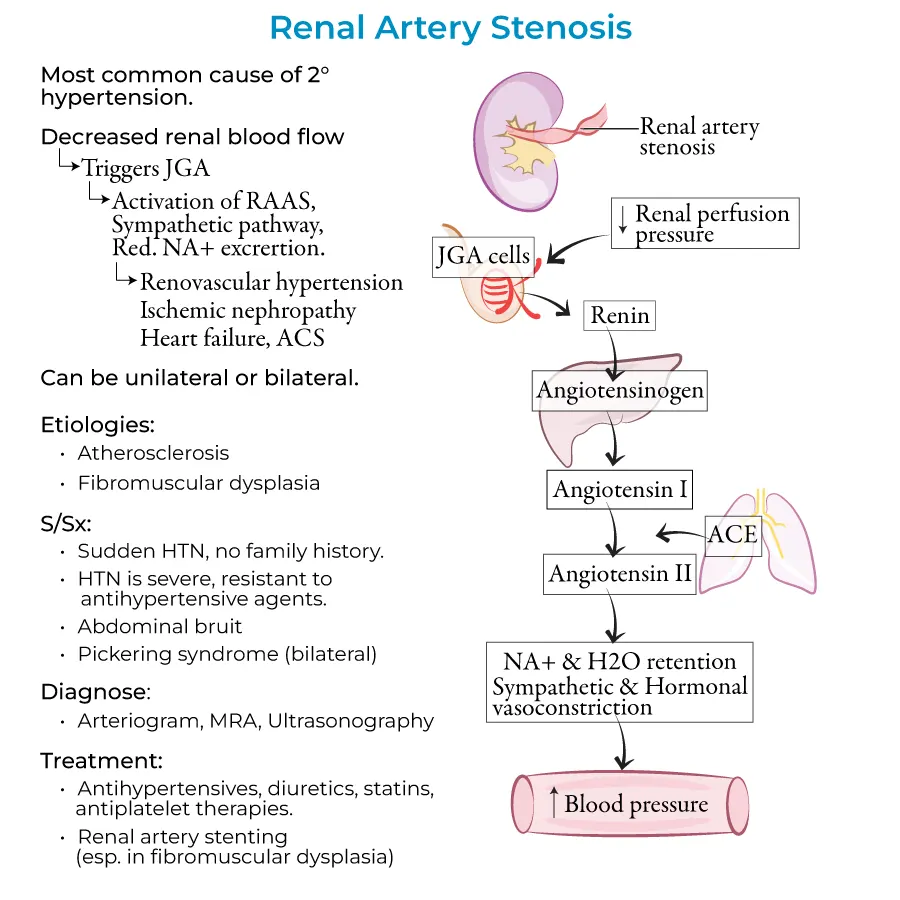
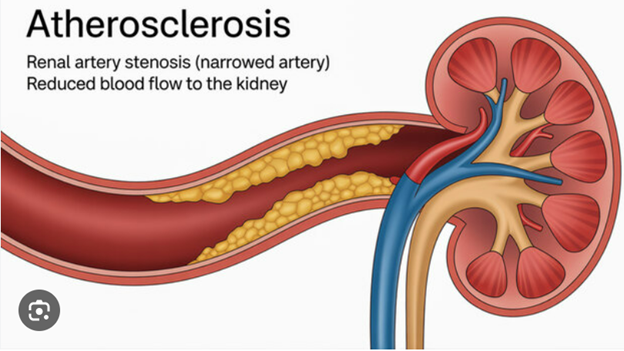
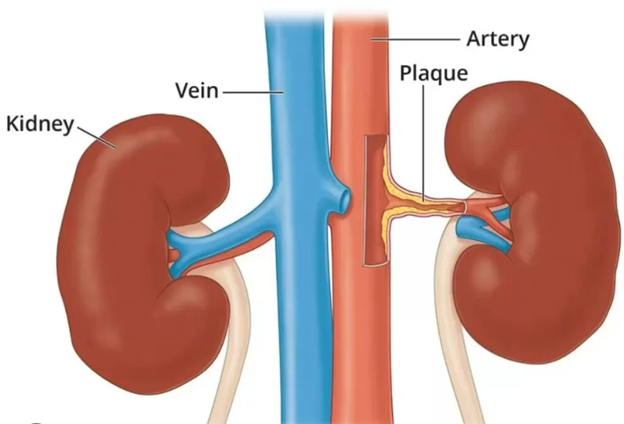
Renal artery disease is the narrowing or blockage of one or both arteries that supply blood to the kidneys. When these arteries become narrowed, the kidneys receive less blood flow and mistakenly signal the body to raise blood pressure, leading to a condition called renovascular hypertension.
Common causes include:
- Atherosclerosis – plaque buildup in older adults, often with other vascular disease
- Fibromuscular dysplasia (FMD) – an abnormal growth of artery walls, more common in younger women
At Vascular Clinic, we help you understand how this vascular condition impacts your blood pressure and kidney health. We use simple explanations and visuals to make the diagnosis less intimidating and easier to grasp.
When to Suspect Renal Artery Disease
Patients may have:
- Difficult-to-control blood pressure, requiring multiple medications
- Worsening kidney function without another clear cause
- Sudden episodes of fluid overload or pulmonary edema
- A bruit (abnormal sound) heard over the abdomen during physical exam
- Invasive angiography (in select cases) to visualize and treat in one setting
These findings may prompt further vascular evaluation.
How We Diagnose Renal Artery Narrowing
At Vascular Clinic, we use advanced, noninvasive imaging and functional assessments to evaluate blood flow to the kidneys:
- Renal artery duplex ultrasound to assess velocity and signs of narrowing
- CT angiography (CTA) to map renal artery anatomy
- Kidney function scans to evaluate how well each kidney is working
- Blood tests to monitor renal function and electrolyte balance
We correlate these findings with your clinical picture to determine if treatment is needed.
Do All Renal Artery Narrowings Require Treatment?
No. Many cases can be managed with medications alone, especially if blood pressure and kidney function remain stable.
However, intervention may be recommended if you have:
- A significant narrowing (typically >60–70%)
- Resistant hypertension not controlled with medications
- Worsening kidney function from impaired perfusion
- Flash pulmonary edema triggered by blood pressure fluctuations
We only recommend procedures when evidence supports a clear benefit—your safety and outcomes come first.
Treatment: Renal Artery Stenting
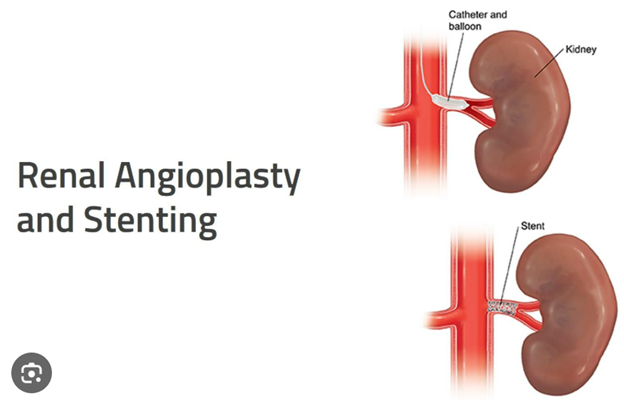
When intervention is appropriate, we offer minimally invasive renal artery stenting—a catheter-based procedure to restore blood flow to the kidney.
How It Works:
- A small puncture is made in the groin
- A catheter is guided to the renal artery under imaging
- A balloon is inflated to open the artery (angioplasty)
- A stent (metal mesh tube) is placed to keep the artery open
Key Benefits:
- Performed under local anesthesia and mild sedation
- No general anesthesia required
- Same-day discharge or 1-night stay
- Minimal discomfort and rapid recovery
- Often results in better blood pressure control and kidney stabilization
Treatment/Combination Explanation

What to Expect
Before the Procedure:
- Imaging review and lab work
- Detailed consultation during your clinic visit
- Clear explanation of risks, benefits, and what to expect
During the Procedure:
- Local numbing and light sedation
- Catheter placement under X-ray guidance
- Real-time assessment of blood flow restoration
After the Procedure:
- Monitoring of blood pressure and kidney function
- Follow-up ultrasounds to ensure the stent remains open
- Clinic visits and lab work to adjust medications as needed
When intervention is appropriate, we offer minimally invasive renal artery stenting—a catheter-based procedure to restore blood flow to the kidney.
Frequently Asked Questions
Will my blood pressure return to normal after the stent?
Many patients see significant improvement, but results vary. Some can reduce medications; others gain stability of kidney function or fewer blood pressure spikes.
Is the procedure painful?
No. It’s performed with local anesthesia and sedation. Most patients feel only mild pressure or soreness at the groin access site.
What happens if I have FMD instead of plaque?
FMD often responds well to balloon angioplasty alone, sometimes without a stent. We tailor the approach based on your artery’s anatomy and condition.
What if I don’t need a stent?
If your blood pressure and kidney function are stable, we recommend medical therapy and regular surveillance with serial imaging and clinic visits.
Why Choose Vascular Clinic?
- Experienced in Renal Artery Stenting and Complex Hypertension Cases
- Minimally Invasive First Approach
- Collaborative Care with Nephrologists and Primary Physicians
- Clear Explanations and Evidence-Based Decisions
- Long-Term Monitoring and Support
We understand the frustration of difficult blood pressure. At Vascular Clinic, our goal is to provide safe, effective treatment that improves your quality of life, with ongoing follow-up to protect both your heart and kidneys.