What Is Pelvic Congestion Syndrome?
Pelvic Congestion Syndrome (PCS) is a condition caused by dilated, dysfunctional veins in the pelvis, most commonly the ovarian veins, that become stretched and engorged under pressure. It primarily affects women of childbearing age, especially those who have had multiple children.
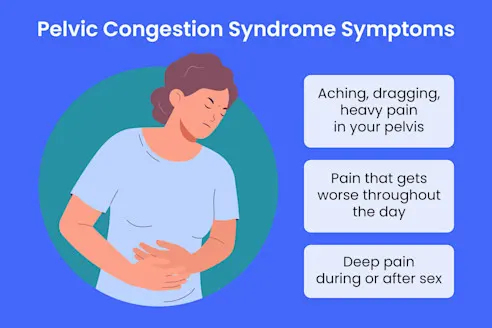
These pelvic varicose veins can cause:
- Chronic, dull pelvic pain or heaviness
- Pain that worsens after standing, during or after intercourse, or around menstrual cycles
- Visible varicose veins on the buttocks, vulva, or upper thighs
- Urinary urgency or discomfort from congested veins pressing on the bladder
Many women suffer with PCS for years, dismissing it as “normal,” but at Vascular Clinic, we want you to know: this pain is real—and it’s treatable.
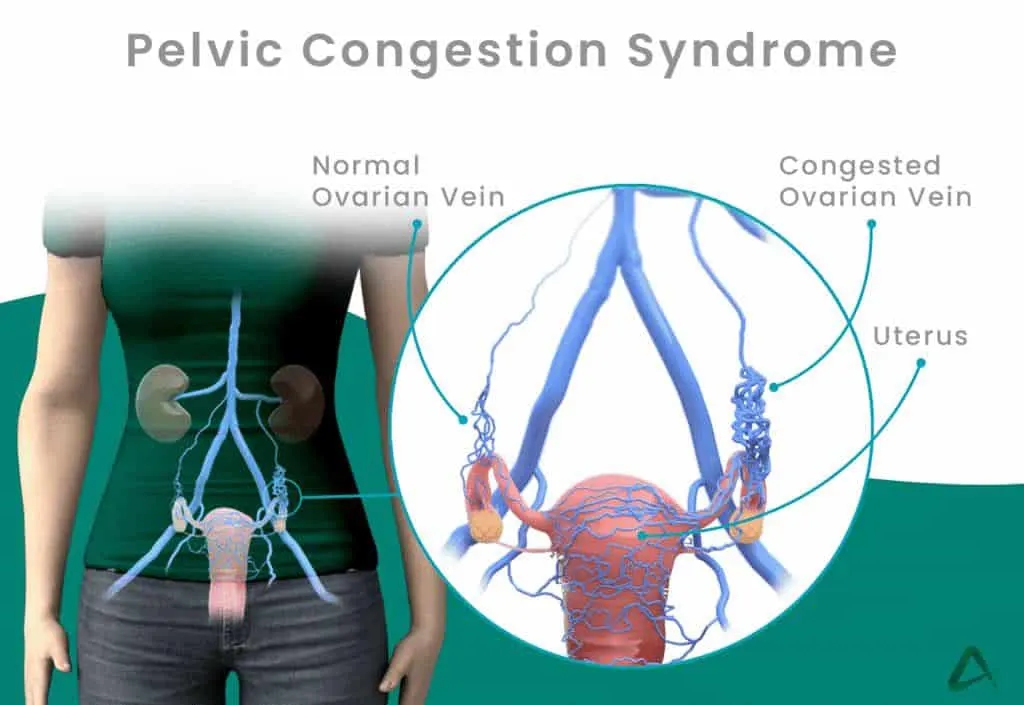
Understanding the Cause
We often explain PCS using the analogy of leaky pipes. Just like in varicose veins of the legs, the one-way valves in pelvic veins fail, allowing blood to flow backward and pool. This increases pressure and causes surrounding veins to stretch and cause discomfort. Our compassionate approach ensures that you feel heard and understood, especially when discussing symptoms that may be personal or difficult to describe.
How We Diagnose Pelvic Congestion
Diagnosis begins with a thorough history and physical exam, followed by non-invasive imaging, including:
- Pelvic ultrasound
- Pelvic MRI or MR venography
- CT venography in select cases
A hallmark feature of PCS is pain that improves when lying down and worsens throughout the day—often a clue that gravity is contributing to venous pooling.
Minimally Invasive Treatment: Gonadal (Ovarian) Vein Embolization
If PCS is confirmed and causing significant symptoms, we treat it with a nonsurgical, catheter-based procedure called gonadal vein embolization.
How It Works:
- A tiny catheter is inserted into a vein in your groin or neck
- Under X-ray guidance, we navigate to the affected ovarian veins
- Tiny metal coils or sclerosant foam can be used to seal off the malfunctioning veins
- Blood flow is rerouted to healthy veins, relieving congestion and pressure
Procedure Details:
- Performed with local anesthesia and light sedation
- No surgical incisions, just a needle puncture
- Typically takes 1–2 hours
- You go home the same day
- Resume normal activities within 1–2 days

What to Expect After the Procedure
- Symptom improvement begins within weeks and continues for months as the veins decompress
- You may experience mild pelvic cramping or low back discomfort (post-embolization syndrome) for a few days
- We prescribe medication as needed for comfort
- Follow-up clinic visits and imaging track your progress
Most patients report:
- Less pelvic heaviness or aching
- Improved exercise tolerance
- Relief from discomfort during intimacy
- Less visual discomfort from pelvic or leg varicosities
Frequently Asked Questions
Is PCS common?
Yes particularly in women who’ve had multiple pregnancies but it is often underdiagnosed because the symptoms can overlap with other conditions.
Will this procedure cure my pain?
Many women experience significant improvement, although some require follow-up treatment or have multiple contributing veins addressed.
Is surgery ever needed?
Rarely. Gonadal vein embolization is successful in the vast majority of cases. If anatomy is unusual or symptoms persist, we’ll discuss further options.
Will I need time off work?
Most women return to normal activity within 24–48 hours, with little restriction.
Why Choose Vascular Clinic?
- Experienced Physicians in Pelvic Venous Disorders
- Advanced Imaging and Targeted Interventional Techniques
- Comfort-Focused Sedation and Same-Day Procedures
- Whole-Person Care for a Sensitive and Often Overlooked Condition
- Clear Communication and Gentle Follow-Up
We don’t just treat veins we help restore your comfort, mobility, and quality of life. You are not alone, and PCS is not something you have to live with.