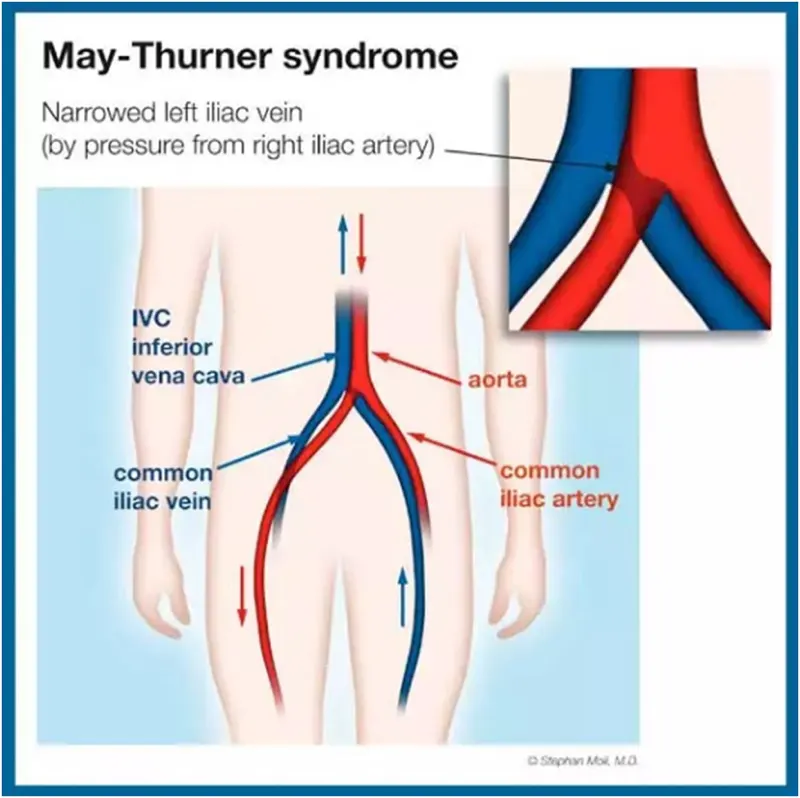
What Is May-Thurner Syndrome?
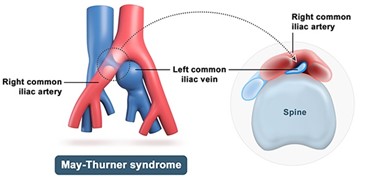
May-Thurner Syndrome (MTS) is a condition where the left iliac vein (which drains blood from the left leg) is compressed by the overlying right iliac artery, restricting blood flow. This pressure can lead to chronic leg swelling, pain, and in some cases, deep vein thrombosis (DVT).
Common symptoms include:
- Left leg swelling (often worse at the end of the day)
- Heaviness, aching, or throbbing in the leg
- Visible varicose veins or skin changes
- History of a left lower extremity DVT
- Discomfort worsens with standing or sitting
The condition is often underdiagnosed, as it mimics other vascular and orthopedic issues. At Vascular Clinic, we specialize in recognizing and treating this often-overlooked vascular compression.
Traditional Evaluation and Treatment Approaches
If May-Thurner is suspected, traditional pathways often include:
- Anticoagulation (Blood Thinners)
- Used if a DVT has formed
- Drawback: While blood thinners prevent new clots, they don’t relieve the underlying vein compression
- Compression Stockings
- Help manage swelling
- Drawback: Provide symptom relief but don’t correct the anatomical cause
- No Treatment (Missed Diagnosis)
- Many patients are told they have “idiopathic swelling” or “post-DVT syndrome” when in fact, MTS is the root cause
At Vascular Clinic, we go further we identify the source of compression and offer targeted, long-term solutions.
How We Treat May-Thurner Syndrome at Vascular Clinic
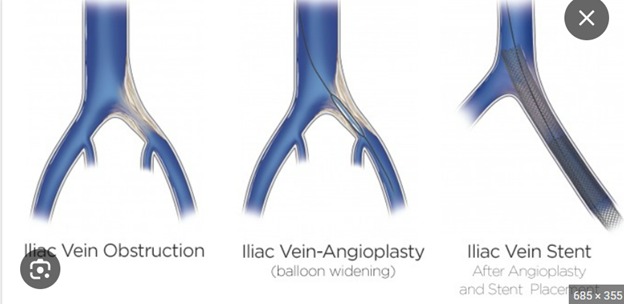
Iliac Vein Stenting
- The most effective modern treatment for MTS is endovascular stenting—a minimally invasive procedure to open the compressed vein and restore normal blood flow.
How the Procedure Works
- Performed under local anesthesia and light sedation
- We insert a catheter through a small puncture in the groin or neck
- We perform a venogram and intravascular ultrasound (IVUS) to visualize the vein narrowing
- Blood flow is restored, relieving pressure and preventing future clot formation
- A self-expanding stent is placed in the compressed iliac vein to hold it open permanently
This procedure does not require open surgery and is typically completed in 1–2 hours, with patients going home the same day.
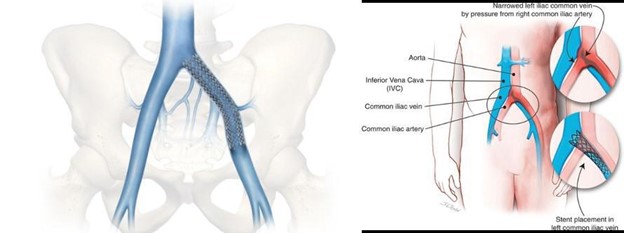
What to Expect After Stenting
- Immediate improvement in venous blood flow
- Swelling and discomfort begin to improve over days to weeks
- Most patients return to normal activities within 24–48 hours
- If you’ve had a prior DVT, we may continue blood thinners temporarily
- Follow-up visits include ultrasound and clinical exams to ensure the stent remains open
Results and Safety
- Iliac vein stenting has a high success rate in resolving symptoms of MTS
- Durable symptom relief in patients with chronic swelling, post-DVT syndrome, or unexplained leg heaviness
- Low risk of complications when performed by experienced vascular specialists
- If stents are placed correctly, long-term patency is excellent
Frequently Asked Questions
How is MTS diagnosed?
We use a combination of venous ultrasound, CT or MR venography, and intravascular ultrasound (IVUS) during the procedure to confirm the diagnosis.
Is the stent permanent?
Yes. The stent remains in place to keep the vein open and prevent recurrence of symptoms.
Can MTS cause a DVT?
Absolutely. The chronic narrowing of the iliac vein increases the risk of deep vein thrombosis, especially in young women or after surgery or travel.
Is this covered by insurance?
Yes. Iliac vein stenting for May-Thurner Syndrome is considered a medically necessary procedure when symptoms or clotting history are present.
Why Choose Vascular Clinic?
- Board-Certified Vascular and Endovascular Experts
- In-house imaging with IVUS and venography for precise diagnosis and treatment
- Minimally invasive care with no large incisions
- Collaborative approach with hematology and primary care teams when anticoagulation is needed
- Compassionate follow-up to ensure symptom resolution and stent durability
At Vascular Clinic, we don’t just manage your symptoms—we resolve the root cause of your leg swelling and clot risk. If you’ve been told it’s “just venous insufficiency” or “just post-DVT,” it might actually be May-Thurner Syndrome—and we can help.